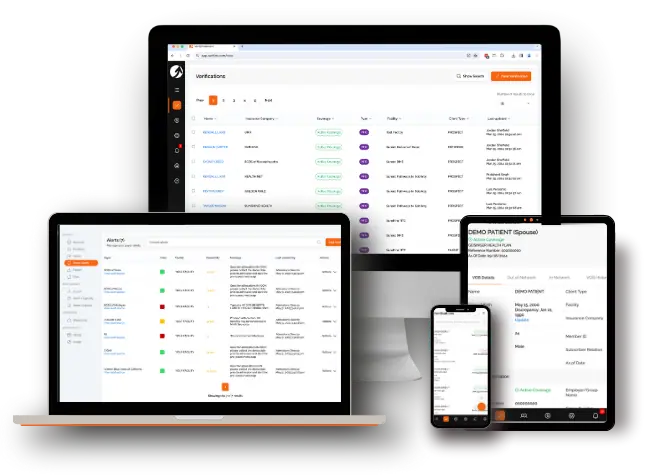
Verification of Benefits Platform
- Instant Verification
- Continuous Coverage Monitoring
- Effortless Team Collaboration
- Month-to-month Flexibility
- Instant Verification
- Continuous Coverage Monitoring
- Effortless Team Collaboration
- Month-to-month Flexibility
And so much more...
- Largest Payer Database in the Industry
- 24/7/365 Web and Mobile App Access
- Custom Web Forms for Lead Generation
- Unlimited User Accounts at No Additional Cost
- Dedicated Customer Support and Unlimited Training
- Seamless Integration
2-Minute Interactive Tour
See for yourself how easy it is to verify benefits instantly!
Need more insight? Request a customized demo with our sales team.
Even More Features to Support Your Patient Admissions Process!
Payer Alerts
Bulk Imports
Patient Claim Status
Full Access APIs
Custom Coverage PDF Export
Seamless HIPAA Compliant Communication
Dedicated Customer Support and Unlimited Training
Setting you up for success from day one is our mission at VerifyTreatment. You’ll have all the resources and personalized guidance you need to ensure you get the most out of our platform.
FAQs—Learn More about the #1 Verification of Benefits Platform
Great question. Legacy verification of benefits methods are limited:
- Limited information – limited number of carriers accessible electronically & limited or inaccurate information.
- Limited mobility – We have an app for smart phone, so you can verify benefits from anywhere.
- Limited functionality – VerifyTreatment is easy-to-use, easy-to-understand, AND we automate the re-verification, which traditionally can take days to accomplish.
Our Solution: We access 1700+ insurance company databases, and provide the most comprehensive electronic VOB on the market.
We check the major insurance carriers (Aetna, BCBS, Cigna, Humana, United), as well as UMR, Oxford, Meridian, Molina, OptimaHealth, Priority Health, Medical Mutual, Preferred One, Qualcare, Amerihealth, UPMC, GHI, Core Source, GEHA, Healthsmart, Harvard Pilgrim, Health Alliance, Health Net, and more!
If VerifyTreatment does not provide all of the required information, use it for nights/weekend VOBs, mobile access, re-verification, and insurance carriers you can’t check using you’re current methods.
We tie in directly with the insurance companies. You input the information, VerifyTreatment accesses the insurance company, and the insurance provides the result. The data provided is directly from the insurance companies’ database.
Key benefit information. Policy status, policy type, deductible/out of pocket amount, met, and remaining, co-insurance, co-pays, plan name, payer notes.
Given the sensitive nature of our business, we take HIPAA compliance and security very seriously. VerifyTX was designed with SSL 128-bit encryption. Your data is treated with bank-like security; encrypted at all times and regularly backed up. By using the service, all users agree to our business associate agreement.
Account creation takes a few moments, and quick personalized training is offered at your convenience. Contact us via email or set up your account today.
Yes, absolutely! Every person that calls your center for help matters, and it’s very important to make decisions fast. Let us show you how you can admit more clients, faster and easier.
Yes, you can access your NPI here – npiregistry.cms.hhs.gov
Yes; VerifyTX is able to check ACA policies.
We provide the information the insurance company provides to us. We are always open to your feedback, contact us at support@verifytx.com.
Sometimes verifications fail to get a result. If this happens, double-check to make sure all of the information has been entered correctly and the information is accurate. You only use credits for successful transactions. We are here to help. Contact us at support@verifytx.com.
Yes, the guide is located within the app and available to your team 24/7. If you need an account, contact us at info@verifytx.com, and we’ll be happy to get you onboarded.





